Viral Vector Production for Biomedicine: Key Applications and Industry Trends
Viral vector production is revolutionizing biomedical science by enabling precise gene delivery methods, which hold promise in treating genetic diseases and developing vaccines (Bulcha et al., 2021). While the concept behind these therapies is relatively simple, they pose significant technological and production challenges which limit their translation to the clinic. This article will cover the applications, technological advancements, and ongoing challenges in viral vector production, highlighting automation as an essential component of modern production workflows.
What is Viral Vector Production
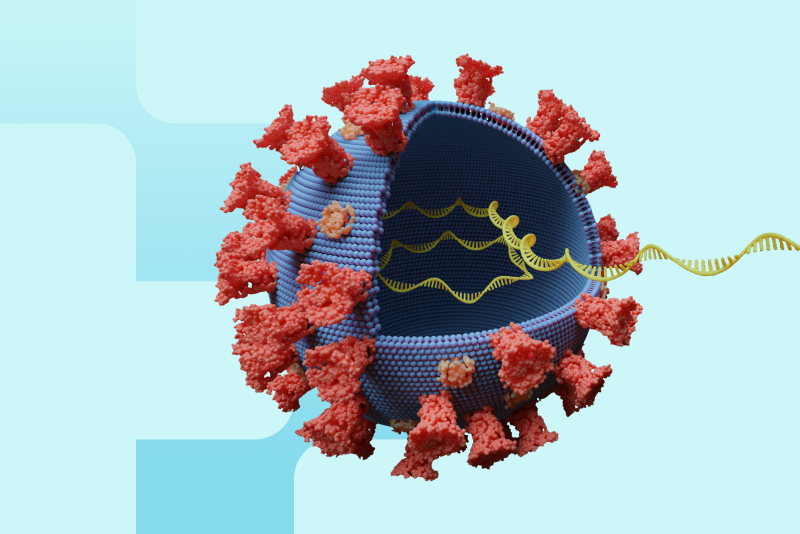
Scientists have been taking advantage of viruses’ unique ability to efficiently introduce genetic material into host cells for decades (Finer & Glorioso, 2017). Delivery methods such as adeno-associated viruses (AAVs) have now become more mainstream in dealing with various diseases, including genetic disorders (Fig. 1). Viral vector production involves generating large quantities of viral vectors containing therapeutic genetic material such as corrective copies of genes or instructions for making an antigen. Generating clonal cell lines that produce these vectors is becoming an essential component of modern biomedicine and requires complex production workflows. Viral vectors have broad applications as clinical tools to treat diseases, including cancer and neurodegenerative disorders (Bulcha et al., 2021).

Key Applications
Viral vectors are now used to treat different diseases and are particularly prevalent in the therapeutic areas of gene therapies and vaccines. The hundreds of current clinical trials currently underway are a testament to the promise of these therapies in addressing genetic disorders, cancers, and infectious diseases (Wang et al., 2024).
Gene Therapy
These therapies involve delivering a corrective gene to tissues impaired by a harmful genetic mutation, introducing gene-silencing mechanisms, inactivating specific genes, or adding a “foreign” gene to enhance cellular function. Gene therapy vectors are administered either directly into patient tissue (in-vivo) or into patient cells or donor cells (ex-vivo), which are then reintroduced. These therapies hold significant promise for treating diseases with well-defined genetic origins, such as cystic fibrosis and muscular dystrophies and many are already under clinical investigation or approved (Bulcha et al., 2021).
Vaccines
Viral vectors are used to deliver genetic information encoding antigens that train the body’s immune system to attack specific pathogens. In recent years, several of these types of vaccines have been approved to combat COVID-19. Viral vector vaccines have also shown potential for addressing a wide range of other infectious diseases, including Ebola (Travieso et al., 2022).
Technological Advances
Several technological advances in recent years have helped streamline the development of viral vectors for applications in biomedicine.
Gene Editing and In-silico Techniques
Gene editing technologies have enabled scientists to optimize viral vector design for safety and therapeutic effect (Lei et al., 2024). AI has the potential to make predictions about the interaction of viral particles with human tissue, enabling the rational development of more optimal delivery systems (Hasanzadeh et al., 2022).
High-throughput Screening
High-throughput screening has revolutionized the screening of drugs and other therapies for toxicity and therapeutic effects. However, it is also being applied to test the effectiveness of viral vector delivery systems. For instance, screening can be used to test capsid titer and content ratio (Gimpel et al., 2021).
Scalable Production
Viral production pipelines have suffered from a lack of scalability. Researchers are increasingly shifting from adherent cell culture to suspension culture, which allows for greater scalability and brings speed and cost efficiencies to viral vector production. This move also reduces the chances of batch-to-batch variation and brings viral vector production processes more in line with other large-scale production processes like those used for monoclonal antibody production (Ansorge et al., 2019).
Automation
Automation carries several advantages wherever it is implemented across viral vector production workflows. By removing a significant amount of risk due to human error and variation, automation helps to streamline production and promotes reproducibility. Automation in liquid handling enables more reliable single-cell seeding, which reduces the chance of contamination from other clones and microbes. Automated cell culture with real-time monitoring ensures cells are maintained at optimal growing conditions, facilitating faster scaling up and less risk to workflows (Holland & Davies, 2020).

Challenges and Future Perspectives
The increased demand for AAV-based viral vectors for gene therapies has highlighted the need for faster, more cost-efficient production methods paired with heightened safety and regulatory compliance. Perennial issues, such as immunogenicity and targeting of viral vectors to appropriate tissues, limit their translational impact. Advances in targeting promise to increase the specificity of viral vectors for specific tissues and cell types (Srivastava et al., 2021; Zhang et al., 2016), while methods including capsid modification with polyethylene glycol (PEG) are helping to reduce the immunogenicity of gene therapy vectors (Kreppel & Hagedorn, 2021).
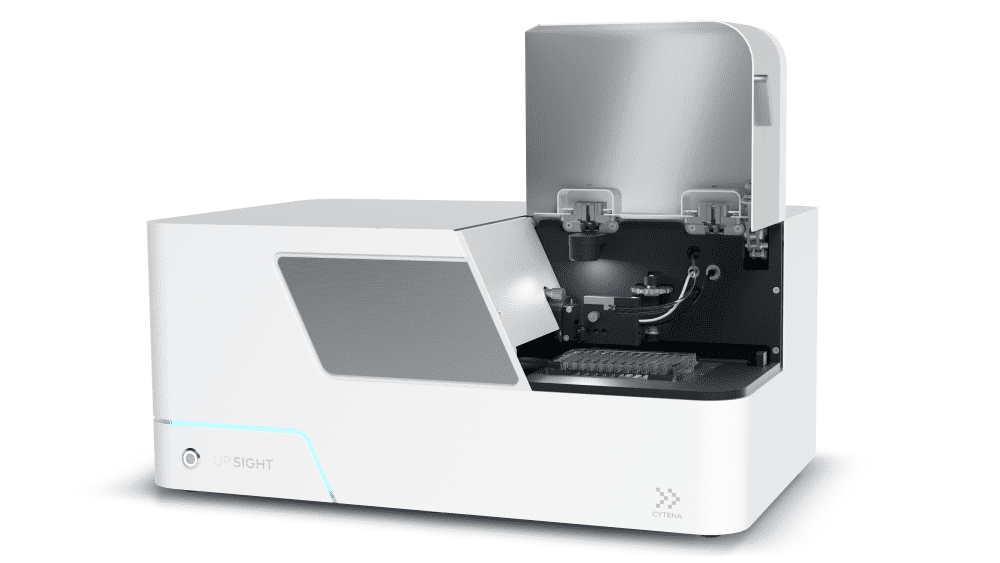
Regulatory bodies require proof of clonality for cell lines used to produce therapeutics, which is challenging to prove using manual cell seeding methods. The UP.SIGHT single-cell dispenser and dual-imager from CYTENA images cells as they are dispensed and after they settle in the well, making it simple to prove clonality to regulators (Fig. 3).
Conclusion
Viral vector production stands at the forefront of therapeutic innovation, enabling groundbreaking advances in gene therapy and vaccine development. CYTENA’s UP.SIGHT technology supports these efforts by enabling regulatory compliance through accurate single-cell seeding. As demand for viral vectors grows, ongoing technological advancements will be essential in meeting safety, scalability, and precision requirements, bringing promising treatments closer to patients worldwide.
CYTENA drives the future of viral vector production by enabling researchers to streamline their processes while ensuring regulatory compliance. Get in touch with our team today to learn more about the UP.SIGHT. Why not book a demo and see how the UP.SIGHT works firsthand?
References
- Ansorge, S., Burnham, M., Kelly, M., McDermott, R., & Jones, P. (2019). Scale-up considerations for improved yield in upstream viral vector production. Cell and Gene Therapy Insights, 5(12), 1719–1725.
- Bulcha, J. T., Wang, Y., Ma, H., Tai, P. W. L., & Gao, G. (2021). Viral vector platforms within the gene therapy landscape. Signal Transduction and Targeted Therapy, 6(1), 53.
- Finer, M., & Glorioso, J. (2017). A brief account of viral vectors and their promise for gene therapy. Gene Therapy, 24(1), 1–2.
- Gimpel, A. L., Katsikis, G., Sha, S., Maloney, A. J., Hong, M. S., Nguyen, T. N. T., Wolfrum, J., Springs, S. L., Sinskey, A. J., Manalis, S. R., Barone, P. W., & Braatz, R. D. (2021). Analytical methods for process and product characterization of recombinant adeno-associated virus-based gene therapies. Molecular Therapy. Methods & Clinical Development, 20, 740–754.
- Hasanzadeh, A., Hamblin, M. R., Kiani, J., Noori, H., Hardie, J. M., Karimi, M., & Shafiee, H. (2022). Could artificial intelligence revolutionize the development of nanovectors for gene therapy and mRNA vaccines? Nano Today, 47, 101665.
- Holland, I., & Davies, J. A. (2020). Automation in the Life Science Research Laboratory. Frontiers in Bioengineering and Biotechnology, 8, 571777.
- Kreppel, F., & Hagedorn, C. (2021). Capsid and Genome Modification Strategies to Reduce the Immunogenicity of Adenoviral Vectors. International Journal of Molecular Sciences, 22(5), 2417.
- Lei, T., Wang, Y., Zhang, Y., Yang, Y., Cao, J., Huang, J., Chen, J., Chen, H., Zhang, J., Wang, L., Xu, X., Gale, R. P., & Wang, L. (2024). Leveraging CRISPR gene editing technology to optimize the efficacy, safety and accessibility of CAR T-cell therapy. Leukemia.
- Srivastava, A., Mallela, K. M. G., Deorkar, N., & Brophy, G. (2021). Manufacturing Challenges and Rational Formulation Development for AAV Viral Vectors. Journal of Pharmaceutical Sciences, 110(7), 2609–2624.
- Travieso, T., Li, J., Mahesh, S., Mello, J. D. F. R. E., & Blasi, M. (2022). The use of viral vectors in vaccine development. Npj Vaccines, 7(1), 75.
- Wang, J.-H., Gessler, D. J., Zhan, W., Gallagher, T. L., & Gao, G. (2024). Adeno-associated virus as a delivery vector for gene therapy of human diseases. Signal Transduction and Targeted Therapy, 9(1), 78.
- Zhang, C., Yao, T., Zheng, Y., Li, Z., Zhang, Q., Zhang, L., & Zhou, D. (2016). Development of next generation adeno-associated viral vectors capable of selective tropism and efficient gene delivery. Biomaterials, 80, 134–145.